Evolving digital capabilities allow healthcare providers to develop better, more personalized care for patients. While the fascinating technological advances are fun to talk about (care to implant a microchip of your medical history?), the more pressing side of technology is how it changes human behavior: how technology reframes the process of finding and using healthcare as patients find new ways to get information (and misinformation). Providers have to anticipate these needs. Here’s a start:
Focus on the user’s journey
Understanding the changes in a patient’s journey is mission-critical. The ways in which patients make decisions has completely changed. According to an article first published in the Harvard Business Review on the new CEO-CMO allliance, people use an average of six different channels to make a purchase decision. They do more comparison shopping, they self-diagnose more, and seek the opinions of others as never before — simply because the technology allows them to do so.
Patient acquisition is changing
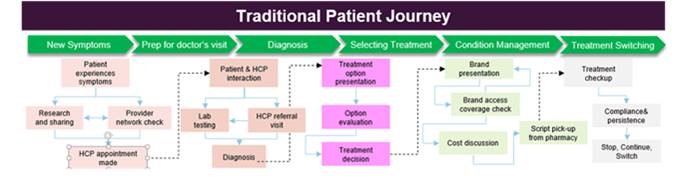
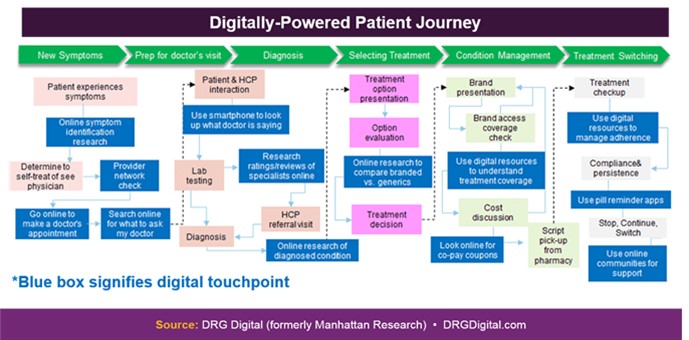
So where do you start if you’re a provider? Let’s start here: DRG Digital diagrammed some of the changes in the patient’s healthcare journey. Here’s the old model, based on the authority and guidance of the provider:
And here’s how digital is interwoven in today’s patient journey:
This model is good as far as it goes, but it leaves out two things. The first is the research into which provider to look to:
The new second opinion
The power of technology to amplify Word of Mouth cannot be underestimated. Google coined the term “ZMOT” or Zero Moment of Truth to describe the feedback structure of consumer choice in the digital age. Experience feedback of one patient becomes the first interaction for the next patient:
In health, communication IS care
Nowhere is feedback more critical than in the healthcare sector, where patient reviews have a direct effect on choice of providers, on hospital’s Medicare reimbursement rates, and even on the risk of litigation: A study by the American College of Preventive Medicine on the importance of communication showed that 71% of patients cite poor relations with their physicians as the cause of malpractice suits. Time-pressured providers need to consider how digital communications can fill in the information gaps that cause non-compliance and misunderstandings.
But let’s talk about an even more crucial aspect that the journey needs to incorporate:
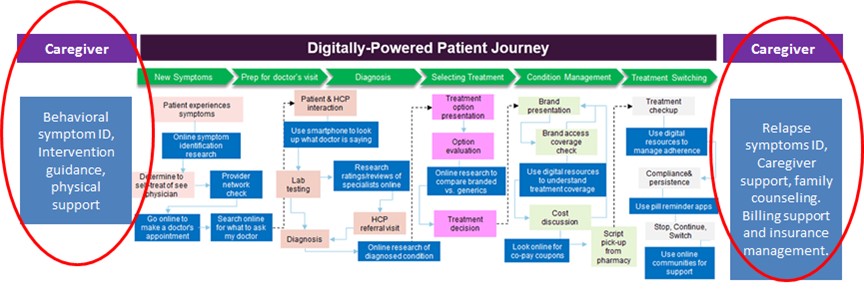
The journey of the caregiver
The journey outlined above is missing a critical piece: Caregivers. For caregivers, the beginning of the process and the concerns of after-care bookend the patient’s care and recovery. Caregivers search for information about symptoms to confirm the seriousness of the behaviors they witness, they seek counseling suggestions, legal guidelines, and agency help in approaching a patient about care. As a patient goes through treatment, they parallel the patient’s search for information about recommended therapies and drugs. Before during and after treatment, they look for signs of remission, ongoing support, billing information and a host of post-treatment information. The Caregiver’s journey includes many of the steps of the patient, but also has actions on either end that are something like this:
Providers must understand and address these stages of engagement (to the extent allowed by HIPPA) to help caregivers support recovery.
Speak into their listening
One of my favorite people, Gail Blanke, taught me the phrase, “Speak into their listening.” It means don’t talk at people — meet them where they are ready to listen.
Provider organizations need to be especially sensitive to the variety of readiness and ability to reach out for help. Not everyone springs up and says, “I need help! Let me call!” Caregivers may recognize a problem before a prospective patient realizes their own need. Patients and caregivers may be concerned about being discovered if they research an issue online. If the patient is a dependent, often one parent recognizes a need before the other, especially in cases of mental health or substance abuse.
So a variety of options is called for. While a provider organization may think their Live Chat feature is a sure thing, young people HATE to speak on the phone, and caregivers may be reluctant to engage with someone who is likely to ask questions they aren’t sure they are ready to answer, or can’t answer without being overheard. A phone call is MUCH MORE of a commitment than an impersonal option to “Get more information” which is more of commitment than reading an infographic with general information. Providing a range of options that lets the patient or caregiver meet you at their stage of readiness will build trust. Asking for personal information too soon can create friction, especially if there is privacy sensitivity.
In today’s marketing world, where a visit to a website may be saved in a PC’s search history, or an ad may retarget an ISP, the risk of discovery can discourage patients seeking information. Mobile contact options that provide discreet communication alternatives such as texting, enhance privacy for those who are reaching out for help in a sensitive situation. North Carolina and other states have had great results with a text-based ‘warm line’ that allows information seekers to get straight forward answers to sensitive questions in a more private setting.
Consider every user touchpoint, including post-care.
Digital channels will continue to change consumer behavior and increase independent decision making. For provider organizations, aligning and managing strategic messages across media channels is essential to providing consistent communication andconsistent care.